Very large health care systems and academic medical centers can employ programmers to create their own LLMs, according to David Kereiakes, managing partner at...
Machine Learning
Previous articles in this series have shown how generative AI can be used for administrative and back-office functions in health care. Now we’ll look at...
The following is a guest article by Vivian Liu, COO at Braid Health One thing in healthcare remains constant: the need for answers. This is why radiology is a...
Previous articles in this series introduced the role of generative AI in the healthcare back office and examined its use in billing and revenue management...
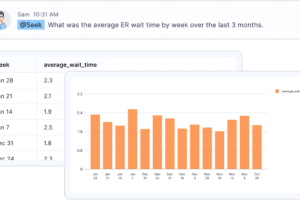
The previous article in this series introduced the topic of generative AI in the back office of healthcare. This article starts to look at healthcare...
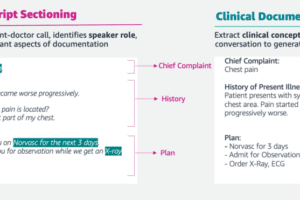
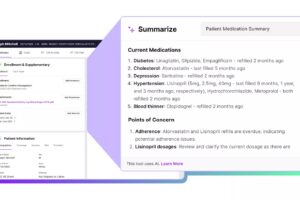
The Healthcare IT Today site has been promoting the use of powerful new capabilities in generative AI for clinical applications, notably the automatic...
The following is a guest article by Archie Mayani, Chief Product Officer at GHX Artificial Intelligence (AI) has been a game-changer in various industries, but...
The following is a guest article by Morris Panner, President at Intelerad Medical Systems By 2034, the U.S. could face a shortage of up to 124,000 physicians...
The following is a guest article by Holly Miller, President at Collette Health (formerly MedSitter) Amid the many challenges in healthcare, an emerging central...
The Partnership Elevates Evidence-Based Business Intelligence for Cost Savings, Efficiencies, and Quality Improvements BurstIQ, a trusted leader in data-driven...